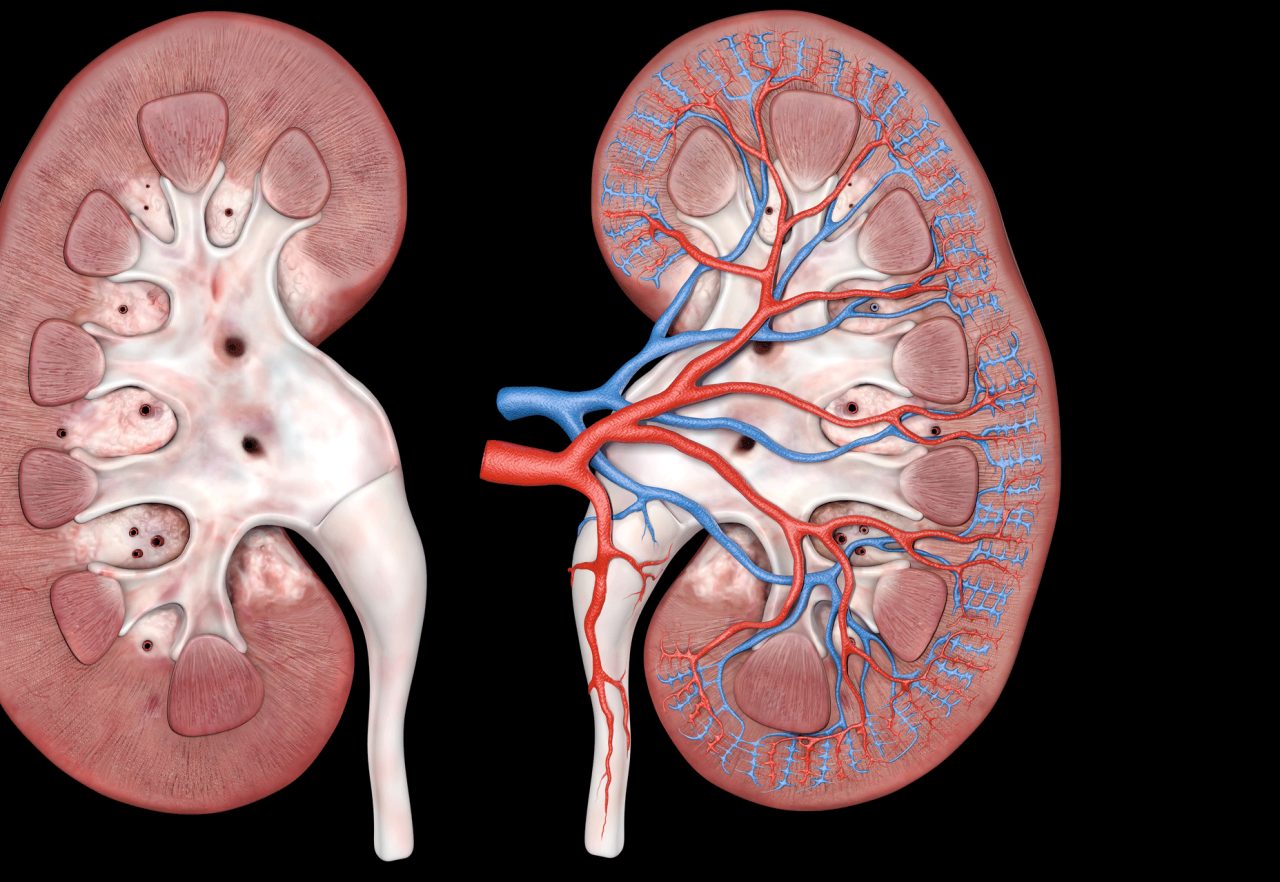
Diabetes and kidney disease often coexist, creating a complex health challenge that requires careful dietary management. Approximately 30–40% of diabetic patients develop diabetic kidney disease (DKD), a leading cause of end-stage renal disease (ESRD). Diet plays a pivotal role in managing blood glucose, protecting kidney function, and preventing complications. This article explores evidence-based dietary approaches for diabetic patients with kidney disease, offering practical strategies to balance nutrition, control symptoms, and improve quality of life.
Understanding the Dual Challenge
Diabetic kidney disease arises when chronic high blood sugar damages the kidneys’ filtering units, impairing their ability to remove waste and regulate fluids. Patients face a dual challenge: controlling blood glucose to manage diabetes while limiting nutrients like protein, sodium, potassium, and phosphorus to protect kidney function. Poorly managed diets can accelerate kidney damage, increase cardiovascular risk, and worsen glycemic control. A tailored dietary plan, guided by a registered dietitian, is essential to address these complexities.
Key Nutritional Goals
Dietary approaches for diabetic patients with kidney disease focus on four primary goals:
- Glycemic Control: Maintaining blood glucose levels within target ranges (typically 70–130 mg/dL fasting) to reduce stress on the kidneys.
- Kidney Protection: Limiting nutrients that strain kidney function, such as protein, sodium, and phosphorus.

- Cardiovascular Health: Reducing risks of heart disease, a major concern for DKD patients, through low-sodium, heart-healthy fats, and controlled calorie intake.
- Nutritional Adequacy: Ensuring sufficient calories and nutrients to prevent malnutrition, a risk in restrictive diets.
Read more: Navigating Hearing Aid Insurance: Costs, Coverage, and Savings Strategies
Protein Management
Protein intake is a cornerstone of dietary management but requires careful balance. Excessive protein can overburden the kidneys, while insufficient protein may lead to muscle loss and malnutrition.
-
Recommended Intake: For early-stage DKD (stages 1–3), the National Kidney Foundation suggests 0.8 g/kg body weight daily, roughly 10–15% of total calories. For advanced stages (4–5) or dialysis patients, 1.0–1.2 g/kg may be needed to prevent malnutrition.
-
Quality Over Quantity: Choose high-quality proteins like egg whites, fish, skinless poultry, or plant-based options (tofu, lentils) to minimize phosphorus and potassium loads. Plant-based proteins are often preferred as they produce fewer uremic toxins.
-
Practical Tip: Spread protein intake evenly across meals to stabilize blood sugar and reduce kidney strain. For a 70-kg person, this might mean 15–20 g of protein per meal, such as a small chicken breast or a cup of cooked lentils.
Carbohydrate Control
Carbohydrates directly impact blood glucose, making their management critical for diabetic patients. However, kidney disease complicates carbohydrate choices due to potassium and phosphorus restrictions.
-
Low-Glycemic Choices: Opt for low-glycemic-index (GI) carbohydrates like whole grains (quinoa, barley), non-starchy vegetables (broccoli, cauliflower), and limited fruits (berries, apples) to stabilize blood sugar. Avoid high-GI foods like white bread or sugary drinks.
-
Portion Control: Use the plate method: fill half the plate with non-starchy vegetables, one-quarter with lean protein, and one-quarter with low-GI carbs. A typical serving might be ½ cup of cooked quinoa or one small apple.

-
Fiber Benefits: Aim for 20–30 g of fiber daily from low-potassium sources like apples, green beans, or whole-grain bread to improve glycemic control and digestion.
-
Practical Tip: Monitor carbohydrate intake (45–60 g per meal, adjusted for individual needs) and pair with protein or healthy fats to slow glucose absorption.
Sodium and Fluid Management
Sodium control is critical to manage blood pressure and fluid retention, common issues in DKD.
-
Sodium Limit: Restrict sodium to 1,500–2,300 mg/day, as recommended by the American Diabetes Association (ADA). High sodium intake can exacerbate hypertension, increasing kidney and cardiovascular strain.
-
Strategies: Avoid processed foods (canned soups, deli meats), use herbs and spices for flavor, and read labels for “hidden” sodium in sauces or snacks.
-
Fluid Intake: In early DKD, fluid needs are typically normal, but in advanced stages or dialysis, fluid restrictions (1–1.5 liters/day) may apply. Monitor urine output and swelling to guide fluid intake.
-
Practical Tip: Replace salty snacks with low-sodium alternatives like unsalted popcorn or fresh vegetables with hummus.
Potassium and Phosphorus Control
Kidney disease impairs the body’s ability to excrete potassium and phosphorus, which can lead to dangerous imbalances.
-
Potassium: Limit to 2,000–3,000 mg/day for advanced DKD. Choose low-potassium foods like apples, berries, green beans, or cabbage over high-potassium options like bananas, oranges, or potatoes. Double-boiling techniques can reduce potassium in vegetables like carrots.
-
Phosphorus: Restrict to 800–1,000 mg/day in later stages. Avoid high-phosphorus foods (dairy, nuts, colas) and processed foods with phosphate additives. Opt for rice milk or fresh meats over processed cheese or sausages.
-
Practical Tip: Work with a dietitian to identify low-potassium, low-phosphorus recipes, such as grilled chicken with steamed green beans and rice.
Fat and Cardiovascular Health
DKD patients face a high risk of heart disease, making heart-healthy fats essential.
-
Healthy Fats: Choose monounsaturated and polyunsaturated fats (olive oil, avocados, salmon) over saturated fats (butter, red meat). Limit trans fats found in fried foods or baked goods.
-
Cholesterol Control: Keep dietary cholesterol below 200 mg/day. Eggs are acceptable if limited to 2–3 yolks per week, focusing on whites for protein.
-
Practical Tip: Incorporate small portions of nuts (e.g., 1 oz almonds, low in phosphorus) or use olive oil for cooking to support heart health without overloading calories.
Micronutrients and Supplementation
DKD patients may need specific micronutrients adjusted:
-
Vitamin D and Calcium: Kidney disease impairs vitamin D activation, so supplements may be prescribed, but avoid excess calcium to prevent vascular calcification.
-
Iron: Anemia is common in DKD; iron-rich foods like lean beef or spinach (in moderation due to potassium) may be recommended, or supplements if prescribed.
-
Practical Tip: Avoid over-the-counter multivitamins unless approved by a healthcare provider, as they may contain excess potassium or phosphorus.
Special Considerations for Dialysis Patients
Dialysis patients have unique dietary needs:
-
Increased Protein: Dialysis removes protein, so 1.2–1.3 g/kg body weight is often recommended. High-quality proteins remain key.
-
Stricter Limits: Potassium, phosphorus, and fluid restrictions are tighter, requiring close monitoring.
-
Practical Tip: Coordinate with a renal dietitian to adjust meals post-dialysis, ensuring adequate calories (30–35 kcal/kg) to prevent weight loss.
Practical Dietary Strategies
-
Meal Planning: Plan meals weekly to balance nutrients. A sample day might include oatmeal with berries for breakfast, a turkey and vegetable wrap for lunch, and grilled fish with quinoa and asparagus for dinner.
-
Portion Awareness: Use measuring tools or visual cues (e.g., a fist-sized portion of rice) to control intake.
-
Regular Monitoring: Track blood glucose, blood pressure, and weight daily, and share results with healthcare providers to adjust the diet.
-
Collaboration: Work with a renal dietitian to create a personalized plan, accounting for stage of kidney disease, diabetes control, and lifestyle.
Challenges and Solutions
-
Dietary Restrictions: The complexity of restrictions can feel overwhelming. Solution: Use apps like MyPlate or Kidney Diet to track nutrients and find compliant recipes.
-
Taste Preferences: Low-sodium, low-potassium diets may seem bland. Solution: Experiment with herbs, lemon juice, or vinegar for flavor.
-
Social Eating: Dining out or family meals can be challenging. Solution: Choose restaurants with customizable options and request low-sodium preparations.
The Role of Lifestyle
Diet is most effective when paired with lifestyle changes:
-
Exercise: Light activities like walking (30 minutes most days) improve insulin sensitivity and cardiovascular health.
-
Weight Management: Maintain a healthy weight to reduce kidney and heart strain, aiming for a BMI of 18.5–24.9.
-
Regular Checkups: Monitor kidney function (eGFR, albuminuria) and HbA1c regularly to assess dietary impact.
Conclusion
Managing diabetic kidney disease through diet requires a delicate balance of controlling blood glucose, protecting kidney function, and supporting overall health. By prioritizing high-quality proteins, low-GI carbohydrates, and heart-healthy fats while limiting sodium, potassium, and phosphorus, patients can slow disease progression and enhance well-being. Collaboration with healthcare providers and dietitians is crucial to tailor these strategies to individual needs. With careful planning and adherence, dietary approaches can empower diabetic patients with kidney disease to lead healthier, more fulfilling lives.








.jpg)


